
The prime of female sexuality occurs at the age of 30-35. But there is the cloud in the silver lining! Starting from the age of 30, contraception may cause unwanted side effects, especially if a woman does not have perfect health, lives in a bit city, does not always lead a healthy lifestyle, and also smokes. Therefore, you should not try every birth control option that a pharmacy offers – you’d better consult a specialist. And first, let’s figure out what inexpensive contraceptives can be used by women in their 30s.
Low-cost contraceptives for women aged 30-39
Pills
First, let’s talk about oral hormonal contraceptives for women after 30 years.
You can take birth control pills of two types:
- Combination (with progesterone and estrogen);
- Progesterone (mini-pills).
The second group is used in cases where estrogen is contraindicated, as well as during breastfeeding. Combination drugs have more and more fans all over the world since they not only prevent pregnancy but also have many beneficial effects on women’s health. Thus, periods become less abundant and less painful, and the risk of cancer decreases.
You cannot choose pills without consulting a doctor. 30-year-old women can have very different hormonal levels, depending on individual indicators. The doctor will tell you what birth control pills to choose – and you’d better consult not only a gynecologist but also with an endocrinologist. After examining the condition of the female organs and hormonal levels, doctors will prescribe one of the following types of contraceptive pills:
- Combination oral contraceptives (also called COCs). They are based on estrogen and progesterone. They are suitable for women who by the age of 30 have decreased lev-els of female hormones or have begun to produce testosterone;
- Mini pills. They contain only progesterone. Most often, they are prescribed to women aged 30 to 50 since they do not contain excess estrogen;
- Low-dose and micro-dose pills. They contain female sex hormones in reduced doses. The doctor will tell you which of these tablets are more suitable than others.
Oral birth control pills can contain the following substances:
- Desogestrel;
- Ethinylestradiol;
- Norethindrone;
- Norgestrel;
- Dienogest;
- Levonorgestrel.
Only the doctor can tell which hormones are better to choose after 30 years.
In particular, to start taking oral contraceptives, you will need to do the following:
- have a blood test, urine test;
- have liver tests;
- check breasts;
- inform the doctor about your heredity;
- undergo gynecological examination;
- check weight, blood pressure.
Low-dose contraceptive pills are recommended for young nulliparous women. They help reduce hairs on the face (antennae) and other parts of the body, normalize weight, and relieve acne. It is better to take high-dose ones after 35 years, to prevent hormonal disruptions in the body after 30 years and to treat them.
Pros:
- The indisputable advantage of birth control pills is their high efficiency – about 99%;
- Oral contraception is suitable for women of virtually any age, including for those aged 30-39. It is only important to choose pills that are suitable for your age category;
- They normalize hormonal levels and reduce the risk of cancer, ovarian cysts, and endometriosis. They also treat mastopathy;
- They make periods regular, make then less painful and less heavy;
- They reduce signs of premenstrual syndrome (PMS);
- They may be used to delay the onset of menstruation ( in this case, a woman should take active pills continuously). This is very useful for women on vacation, on holidays;
- The chances of getting pregnant increase after a certain course of oral contraception for therapeutic purposes;
- After you stop taking the pills, the effect of hormones immediately stops.
Cons:
- Like other medications, oral contraceptives also have some side effects and possible complications;
- There is no 100% guarantee of protection against pregnancy. “Misfires” occur, and this may be due to hormonal disruption in the body, and when missing pills, etc.;
- Taking pills every day at the same time is not always convenient;
- Certain medications reduce the effect of oral contraceptives;
- The pills can cause light spotting in the middle of the cycle. Constant contraception can lead to thinning of the endometrium and complete cessation of the menstrual cycle. This situation requires contacting a gynecologist to exclude a possible pregnancy;
- A serious complication of taking combined oral contraceptives is venous thrombosis and thrombophlebitis. This is especially true for preparations containing a synthetic analogue of progestin – drospirenone. This component of birth control pills can significantly increase the risk of thrombotic complications in comparison with other combined oral contraceptives containing other gestagens;
- Some birth control pills may increase your appetite and retain fluid in your body, leading to weight gain. Therefore, you need to be active and exercise regularly;
- Sometimes oral contraceptives may cause hair loss. Therefore, you should take an additional complex of vitamins and consult a doctor;
- There are other individual unpleasant side effects: bloating, increased blood pressure, breast tenderness, headaches, temporary visual impairment.
Vaginal gel and cream
Unlike hormonal contraceptives, a vaginal gel can be used without consulting a doctor. Spermicides are chemical contraceptives – these are special creams and gel. The dosage form may be different, but the essence is the same: sperm blocking. If everything is done correctly, the method is quite reliable. In addition, antibacterial spermicides can protect against some sexually transmitted diseases. However, not all of them. A condom is safer in this regard.
Spermicides are not as effective as birth control pills – the efficiency is about 80%.
In some cases, a woman and her partner may feel discomfort since spermicides can irritate the mucous membranes and cause allergic reactions. Secondly, not everyone likes when the foam is released from the vagina during intercourse.
Pros:
- Vaginal gel or cream is suitable for women of all ages;
- Spermicidal agents do not violate the vaginal microflora;
- Does not affect menstruation;
- Convenient and easy to use;
- Reduces the risk of contracting sexually transmitted infections;
- Serves as a lubricant.
Vaginal cream or gel can be used together with other types of protection: condoms, intrauterine devices, caps, ring, etc.
Cons:
- There is a risk of getting pregnant. This type of contraception is suitable for couples who trust each other and have irregular sex lives;
- The drug destroys all microorganisms in the vagina, and its frequent use can disrupt the microflora;
- The contraceptive should not be used in the shower or in places with water. In this case, its effect is reduced to zero;
- If intercourse does not occur within an hour, the drug should be re-administered;
- Some women do not respond well to contraception. They may experience irritation and rashes on the mucous membrane.

Shur-Seal Gel Review
- Active Ingredient: Nonoxynol-9
- Release Form: Vaginal Gel
- Age: 18 - 55 years
- Average Price: $30 - $40

Smart Women’s Choice Vaginal Contraceptive Review
- Active Ingredient:
- Release Form: Vaginal Cream
- Age: 18 - 65 years
- Average Price: $55 - $80
Vaginal suppository
Vaginal suppositories are spermicides, that is, not hormonal drugs. They are recommended to be used by women after 30 years who have regular sex life since such suppositories can be inserted into the vagina a few minutes before the onset of sexual intercourse and not be used during the absence of intimate meetings. It should be noted that the degree of protection against unwanted pregnancy in spermicides is somewhat lower than that of hormonal drugs, but they are still quite reliable.
All currently existing contraceptive suppositories are divided by specialists into certain types, in accordance with their composition. Often, modern contraceptives contain only 2 substances:
- Nonoxynol. This chemical substance acts as follows: this element has a somewhat peculiar paralytic effect on spermatozoa. In turn, the cervix begins to produce more mucus, and as a result, spermatozoa cannot enter the uterine cavity at all and, as a result, pregnancy does not occur;
- Benzalkonium chloride. This chemical element has a similar principle of action. It destroys the entire membrane of male sperm cells, and when they enter the fallopian tubes, they are already completely destroyed and, accordingly, lose the ability to naturally fertilize the egg.
Before intercourse, during the time indicated directly in the drug’s instructions, the candle must be inserted as deep as possible into the vagina. On average, the effect of a suppository lasts about 40 minutes. Before each repeated intercourse, it is necessary to introduce an additional 1 more suppository.
Women should remember that all suppositories sold in pharmacies provide only an 80 % guarantee that an unwanted pregnancy will not occur. Thus, there remains about 20% of the likelihood that a woman will still have an unwanted pregnancy after sexual intercourse. Experts say that about 5% of these cases are the woman’s fault, i.e. improper storage of suppositories, or their incorrect use. That is why it is so important that women carefully follow the instructions for using the contraceptive suppository and do not deviate from it a single step.
Note: if a woman has an active sex life, then she should think about choosing another means of contraception. Experts believe that suppositories are more suitable for use with single intercourse when it is simply inappropriate to insert a special intrauterine device and regularly take hormonal pills.
Contraceptive suppositories are considered the right solution for those women who, for whatever reason, have serious contraindications to the use of other contraceptive drugs.
Contraceptive suppositories are good because, in addition to preventing pregnancy, they have a detrimental effect on pathogenic microflora – both viral pathogens and bacterial ones. But a woman should not completely rely on birth control suppositories. Yes, they are antiseptics, but they will not be able to completely protect women from a wide range of sexually transmitted diseases.
Pros:
- In addition to its direct purpose – to protect a woman from unwanted pregnancy, suppositories to some extent are able to protect against diseases, bacteria, and viruses;
- Contraceptive suppositories can provide quite a good service for those women who have problems with the release of lubricant. When lubrication is produced insufficiently, intercourse can be unpleasant. Suppositories can almost entirely solve this problem.
Cons:
- When used regularly, modern contraceptive suppositories can negatively affect the vaginal microflora;
- Birth control pills can cause severe irritation, which entails an inflammatory process of the mucous membrane of the cervix and vagina. As a result, women may experience an uncomfortable itching/burning sensation. It is important to note that the feeling of discomfort over time can lead to the fact that a woman will not only have to forget about sexual intercourse but also urgently see a gynecologist;
- Some women note the fact that using contraceptive suppositories deprives them of those feelings that only the effect of spontaneous intercourse can bring. And this is understandable because women have to accurately calculate the time since the suppository must be inserted into the vagina 5-10 minutes before intercourse, and then – go to bed and start the pleasure of love until the effect of this suppository is over. Agree, discipline does not add pleasure.

Nonoxynol-9 Review
- Active Ingredient: Nonoxynol-9
- Release Form: Vaginal Suppository
- Age: 18 - 55 years
- Average Price: $20
Vaginal ring
Do not confuse a vaginal ring with caps and diaphragms! The vaginal ring is a high-tech product (thin, about 4 cm in diameter) made of silicone and includes a deposited hormonal contraceptive. It does not interfere with sexual activity, it does not create the sensation of a foreign body. The ring is inserted into the vagina on the first day of menstruation and left there for three weeks. All this time, the ring gradually releases the hormones that prevent pregnancy. After 21 days, the ring must be removed for a week.
Pros:
- No effect on the composition of the bacterial microflora of the vaginal mucosa;
- Increased vaginal lubrication;
- Treatment of cervical erosion (with prolonged use);
- Lack of influence on sexual desire, discomfort during sexual intercourse. Some women even increase the frequency and intensity of orgasm;
- Lack of primary passage of hormones through the digestive tract and negative effects on the digestive tract;
- Reliability and a high degree of protection against unwanted pregnancy;
- Ease of use;
- Fast restoration of reproductive function.
Cons:
- Need a preliminary consultation with a gynecologist;
- Like all hormonal contraceptives, the ring has contraindications and side effects;
- When using it, the degree of cleanliness of the vagina should correspond to the norm;
- It is undesirable to use tampons during menstruation.
The hormonal ring is recommended for those who are not able to take pills every day or suffer from gastrointestinal diseases.
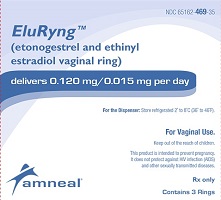
EluRyng Review
- Active Ingredient: Ethinylestradiol / Etonogestrel
- Release Form: Vaginal Ring
- Age: 18 - 45 years
- Average Price: $60.00
Injection
A hormonal injection for three months contains the hormone progestogen in a high dose and delays ovulation for three months. After childbirth, this injection can be given in at least six weeks.
Pros:
- A hormonal injection is one of the most reliable methods of contraception;
- During intercourse, you do not have to think about methods of protection and the injection occurs only a few times a year;
- This method cannot lead to any errors in the use;
- You can also get an injection while breastfeeding.
Cons:
- The hormone contained in the injection can cause unwanted side effects that last as long as the injection itself lasts. In this case, the medication cannot be withdrawn and you will have to wait for the end of three months. Be sure to discuss with your doctor if this method is right for you;
- Concomitant use with other medications should be discussed with your doctor;
- The hormone injection is only given by a doctor.

Provera Review
- Active Ingredient: Medroxyprogesterone Acetate
- Release Form: Pills, Suspension for Injection
- Age: 18 - 45 years
- Average Price: $10

Medroxyprogesterone Review
- Active Ingredient: Medroxyprogesterone Acetate
- Release Form: Pills, Suspension for Injection
- Age: 18 - 45 years
- Average Price: $10
Transdermal patch
The contraceptive patch is also designed for three weeks of use. There are three of them in the package, each designed for a week. The first one is glued to the skin on the first day of your period and is changed after a week. After three weeks, you need to take a seven-day break. Wearing a patch, you can safely visit the bathhouse, the pool – it will not fall off, and no one will notice it – its dimensions are only 2×2 cm, it is flesh-colored, that is, it does not strike the eye. And you can stick it on the shoulders, under the shoulder blade, on the thigh, on the bottom of the belly, on the buttocks. It is important to alternate places.
An important property of both the ring and the patch is that the effectiveness of contraception does not depend on the state of the gastrointestinal tract. The ability to give birth to a child is just as easily reversible as with the use of oral contraceptives. Contraindications are the same as for oral contraceptives.
The hormonal patch is recommended for those who are not able to take pills every day or who suffer from gastrointestinal diseases.
Pros:
- The patch needs to be changed only once a week, in contrast to the pills, which you need to remember to take every day;
- Being late in changing the patch up to 48 hours does not reduce its contraceptive effect;
- In addition to avoiding unwanted pregnancy, the patch stabilizes irregular cycles, reduces menstrual pain, reduces PMS symptoms, and improves skin and hair condition;
- The patch provides a gentle gradual release of the hormone into the body;
- Conflict with other oral medications is excluded;
- The substances contained in the patch stop entering the body as soon as you remove it. This is very important if you have an allergy to any element from the composition.
Cons:
- Side effects – nausea, migraine, drowsiness, increased blood pressure, edema, anxiety (see the full list in the instructions for a particular product);
- The patch can cause skin irritation;
- Restrictions: you cannot use the patch during lactation, smokers, overweight women (over 90 kg), those with thrombosis and diabetes;
- The patch may fall off.

Twirla Review
- Active Ingredient: Ethinylestradiol / Levonorgestrel
- Release Form: Transdermal Patch
- Age: 18 - 45 years
- Average Price: $3

Ethinyl Estradiol / Norelgestromin Review
- Active Ingredient: Ethinyl Estradiol / Norelgestromin
- Release Form: Transdermal Patch
- Age: 18 - 45 years
- Average Price: $30 - $40
Kurvelo Review
Ortho-Cyclen Review
Ortho Tri-Cyclen Review
Jencycla Review
Provera Review
Medroxyprogesterone Review
Ethinyl Estradiol / Norgestimate Review
Errin Review
Sprintec Review
Ethinyl Estradiol / Norethindrone Review
Microgestin 1 / 20 Review
Cryselle Review
AfterPill Review
Rugby Levonorgestrel Tablet Review
Lyza Review
Aviane Review
Morning After Review
Blisovi Fe 1 / 20 Review
Junel Fe 1 / 20 Review
New Day Review
Ovrette Review
Microgestin Fe 1/20 Review
Apri Review
Kelnor 1/35 Review
Tri-Lo-Estarylla Review
Aurovela Fe 1.5 / 30 Review
React Review
Larin Fe 1 / 20 Review
Necon 0.5 / 35 Review
MonoNessa Review
Ortho Novum 1/35 Review
Necon 7 / 7 / 7 Review
Microgestin Fe 1.5/30 Review
Cyred Review
Falmina Review
Levlen Review
Ortho Tri-Cyclen Lo Review
Tri-Lo-Sprintec Review
Gildagia Review
Alesse 21/28 Review
Balziva Review
Gildess Fe 1.5/30 Review
Previfem Review
Incassia Review
Yasmin 28 Review
Tarina 24 Fe Review
Preventeza Review
Yaz Review
Pirmella 7/7/7 Review
Aubra Review
Levonorgestrel Tablets 0.75mg Emergency Contraceptive Review
Zenchent Review
Ortho-Novum 7 / 7 / 7 Review
Opcicon One-Step Review
Lo-Ovral (21/28) Review
My Choice Emergency Contraceptive (Levonorgestrel Tablet 1.5 mg) Review
Iclevia Review
Yasmin 21 Review
Ethinyl Estradiol / Levonorgestrel Review
Loestrin 21 1.5 / 30 Review
Vyfemla Review
Estrostep Fe Review
Estarylla Review
Demulen 1/35-21/28 Review
Jasmiel Review
Chateal Review
Pimtrea Review
Tilia Fe Review
Estrostep 21 Review
Ethinyl Estradiol / Ethynodiol
Azurette Review
Emoquette Review
Zarah Review
Simliya Review
Kariva Review
Reclipsen Review
Ortho-Cept Review
Viorele Review
TriNessa Review
Mircette Review
Tri-Levlen Review
Bekyree Review
Enskyce Review
Kimidess Review
Tri-Sprintec Review
Nora-Be Review
Zovia 1 / 35E Review
Volnea Review
Microgestin 1.5 / 30 Review
Zovia 1/50E Review
Mili Review
Syeda Review
VyLibra Review
Norlyroc Review
Desogen Review
Gianvi Review
EContra EZ Review
Gildess Fe 1 / 20 Review
Junel Fe 1.5 / 30 Review
Loestrin 24 Fe Review
Nylia 7/7 /7 Review
Nikki Review
Junel 1.5/30 Review
Gildess 1/20 Review
Femcon Fe Review
Tarina Fe 1 / 20 Review
Necon 1 / 50 Review
Velivet Review
Tri-Mili Review
Taytulla Review
My Way Emergency Contraceptive (Levonorgestrel Tablet 1.5 mg) Review
Femynor Review
Tri-VyLibra Review
Philith Review
Tri-Legest Fe Review
Loestrin 21 1 / 20 Review
Tri Femynor Review
Lillow Review
Low-Ogestrel-28 Review
Pirmella 1/35 Review
Kelnor 1 / 50 Review
Afirmelle Review
Aurovela 1.5/30 Review
Alyacen 7 / 7 / 7 Review
Aurovela 1/20 Review
Desogestrel / Ethinyl Estradiol Review
Isibloom Review
Aurovela 24 Fe Review
Ortho-Novum 10/11 Review
Tri-Lo-Marzia Review
Loestrin Fe 1 / 20 Review
Necon 10/11 Review
Genora 1/35 Review
Aurovela Fe 1/20 Review
Genora 1/50 Review
Next Choice One Dose Review
Nordette 28 Review
Nortrel 0.5/35 Review
Cyonanz Review
Blisovi Fe 1.5/30 Review
Cyclafem 7 / 7 / 7 Review
Mylan Review
Brevicon Review
Enpresse Review
Hailey 24 Fe Review
Gildess 24 Fe Review
EContra One-Step Review
Zumandimine Review
Junel Fe 24 Review
Trivora-28 Review
Aftera Review
Hailey Fe 1 / 20 Review
Ethinyl Estradiol / Norgestrel Review
Levlite Review
Qlaira Review
Tulana Review
Levonest Review
Lomedia 24 Fe Review
Ayuna Review
Microgestin 24 Fe Review
Sronyx Review
Nexesta Fe Review
Nortrel 7/7/7 Review
Nylia 1 / 35 Review
Delyla Review
Alyacen 1 / 35 Review
Altavera Review
Vienva Review
Tri-Previfem Review
Deblitane Review
Levora Review
Dasetta 1 / 35 Review
Norinyl 1+35 Review
Nortrel 1/35 Review
Norethindrone Review
Portia Review
Larin 1.5 / 30 Review
Tri-Linyah Review
Fallback Solo Review
Next Choice Review
Tri-Estarylla Review
Solia Review
Junel 1 / 20 Review
Camila Review
Trinessa Lo Review
Mestranol / Norethindrone Review
Wera Review
Nor-QD Review
Modicon Review
Plan B Review
Lutera Review
Necon 1 / 35 Review
Lessina Review
Myzilra Review
Juleber Review
Blisovi 24 Fe Review
Cyclafem 1/35 Review
Larin 1/20 Review
Kalliga Review
Caziant Review
Larin Fe 1.5/30 Review
Cesia Review
Elinest Review
Larissia Review
Sharobel Review
Aranelle Review
Norlyda Review
Tri-Norinyl Review
Mono-Linyah Review
Tri-Legest Review
Ulipristal Off Label Review
Heather Review
Ortho-Novum 1/50 Review
Jolivette Review
Leena Review
Beyaz Review
Wymzya Fe Review
Triphasil Review
Ulipristal Review
Option 2 (Levonorgestrel Tablet 1.5 mg) Emergency Contraceptive Review
Plan B One-Step Emergency Contraceptive (Levonorgestrel Tablet 1.5 mg) Review
Dasetta 7/7/7 Review
Ethinyl Estradiol/Folic Acid/Levonorgestrel Review
Kaitlib Fe Review
Loestrin Fe 1.5 / 30 Review
Mibelas 24 Fe Review
Cyclessa Review
Generess Fe Review
Orsythia Review
Take Action Emergency Contraceptive Levonorgestrel 1.5mg Review
Ovral 28 Review
Ogestrel 0.5 / 50 Review
Gildess 1.5 / 30 Review
Marlissa Review
Ethinyl Estradiol / Etonogestrel
Simpesse Review
Ella Review
Ortho Micronor Review
FaLessa Kit Review
Jaimiess Review
Lo-Zumandimine Review
Jenest 28 Review
Amethyst Review
Briellyn Review
Quasense Review
Setlakin Review
Melodetta 24 Fe Review
Drospirenone / Ethinyl Estradiol Review
Ovcon 35 Review
Tri-Lo-Mili Review
Zeosa Review
Ella Review
Ovcon 50 Review
Vestura Review
CamreseLo Review
Zenchent Fe Review
Loryna Review
Lo Simpesse Review
Demulen 1/50-21/28 Review
Amethia Lo Review
Larin 24 Fe Review
Lo Loestrin Fe Review