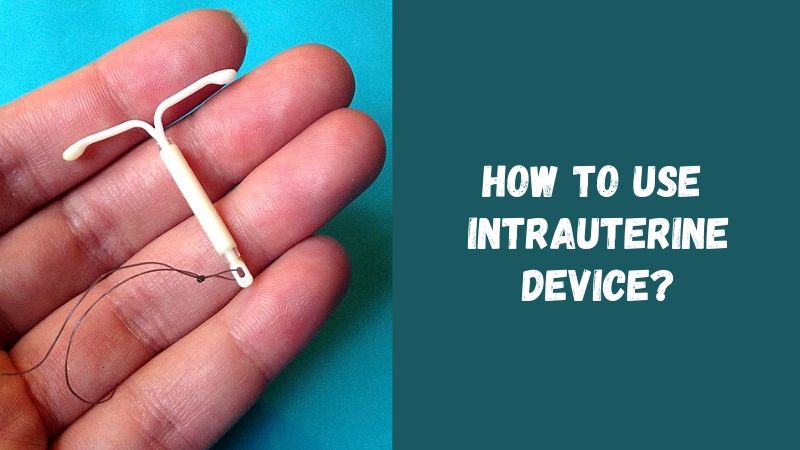
An intrauterine device (IUD) is a small device placed in the uterus in the form of a spiral or letter T with antennae at the ends. The presence of a foreign body in the uterine cavity does not allow the egg to attach and makes it possible to prevent pregnancy.
This phenomenon was discovered a very long time ago by Middle East camel drivers. During long crossings through deserts, they introduced a small stone or pebble into the uterus to the females in order to avoid an unwanted pregnancy. Let’s talk in more detail about the intrauterine device – the types, mechanism of action, and how to use it.
How does IUD work?
There are many IUDs of various shapes and sizes. They are all made of plastic, some have copper or silver thread, others contain a reservoir of progesterone.
It is generally accepted that the IUD causes inflammatory processes and facilitates the penetration of microinjections into the uterine cavity. In order to protect itself, the uterus produces a large number of white blood cells designed to destroy the pathogen, in this case, it is sperm or a fertilized egg.
Irritated by the presence of an IUD, the inner surface of the uterus creates and maintains an environment in constant readiness that is unfavorable for the egg or sperm. The IUD can also contribute to increased mobility of the tubes, which leads to the ejection of the germ cell before being fertilized and doubles the speed of movement of the sperm.
As a result, the level of prostaglandin rises, which does not allow the egg to fix on the walls of the uterus. The copper compound released from copper filaments alters the mucous membrane, making it fatal to sperm.
How effective is IUD? The IUD is in second place after birth control pills. The effect is achieved in 96% of cases. For 100% safety, a woman should also use spermicidal agents.
Is the process reversible? The IUD can have an adverse effect on the female body and its reproductive ability. Its consequences:
- Disease and infection of the pelvic organs;
- Perforation of the uterus;
- Ectopic pregnancy.
However, in most cases, such problems do not arise and residual effects are impossible.
How to insert an intrauterine device?
The introduction of an IUD is a usual medical operation, which is performed in the medical office and does not require anesthesia or special preparation. Nevertheless, in order to identify possible contraindications, it is necessary to undergo a preliminary gynecological examination and have some tests.
If possible, it is also advisable to undergo a clinical examination, talk with the doctor, have a cytobacteriological analysis of vaginal discharge and tissues, and a blood test to identify possible sexually transmitted diseases.
During the first visit, the doctor studies the depth and position of the uterus in order to choose the spiral necessary in a particular case. If the uterus is small or the woman has never given birth, the doctor will insert a small IUD. The doctor indicates the number of the device and the medicine that you need to bring with you for the.operation.
And now this day has come. You are nervous and even afraid. In practice, it turns out that the introduction of the IUD occurs very quickly – in 3 minutes, and is absolutely painless. The doctor inserts a surgical mirror into the vagina, disinfects the cervix and sets the forceps on one of her its lips (there is a slight tingling sensation) to penetrate the cervix to the body of the uterus.
The doctor introduces a small probe through the cervical canal and measures the depth of the uterine cavity (hysterometry) to find out what size of the device should be chosen. Immediately before insertion, the device is placed in a small tube of small diameter. As a result, the device is deformed and becomes stretched like an elastic band.
Now the doctor needs to act very quickly to prevent a change in its shape.
Once the device is inserted, the gynecologist pushes the injected part a few centimeters into the uterine cavity. This makes the IUD take its initial shape.
The doctor carefully removes the pusher and the device for introducing the IUD. The procedure is completed.
Watch a video about how to insert IUD:
This really simple operation can be accompanied by mild, dull pains or simply unpleasant sensations. Women who gave birth in a natural way, consider the introduction of the IUD is absolutely painless. Those who have never given birth or have a very narrow cervical canal are more sensitive. Some women experience painful cramps within minutes.
And finally, there is only a cut of the thread. The penis of a man runs the risk of getting entangled in strings that are too long, and too short strings can prick! The doctor cuts the threads at a distance of 2-3 centimeters from the entrance to the cervix. A woman can feel these strings with her fingers indicating the presence of an IUD.
How to check your IUD strings
Check for the presence of an IUD immediately be-fore the first sexual intercourse (if you do not have the courage, ask your partner to do it); check your IUD strings every time after menstruation, and then from time to time. This can be done with your finger:
- Tighten the feet as close to the buttocks as possible to reduce the length of the vagina;
- Enter the pre-sanitized middle finger. The finger extends the lips of the vagina and touches the con-vex part of the cervix;
- Feel for the hole (small recess) in which the strings are located;
- On certain days, the uterus can move in such a way that it is very difficult to detect the cervix or find a hole.
Try the operation the next day. If you do not feel protruding strings for several days or they appear shorter or longer than they should be, or if you feel the protruding plastic part with your finger, see a doctor.
It is recommended to have a special mirror at home and periodically arrange a self-examination. With its help, you can also check your IUD strings. Usually, a medical examination should be performed a month after the IUD insertion. Then it is recommended to see a doctor every six months.
Possible reaction of the body to the IUD
A woman may get small bleeding without complications. If it does not stop or turns into severe open bleeding, she should consult a doctor. It can be stopped with a simple treatment. Cramping or intrauterine pain may also occur. It can be stopped by antispasmodics prescribed by the doctor.
There is always a risk that IUD falls out. For this, self-observation is recommended. The body has a unique ability to reject a foreign body. If it does not tolerate the device, then rejection will occur within the first three months. Often this occurs during menstruation. Sometimes a woman does not notice that the IUD has fallen out.
Carefully observe yourself and pay attention to the bottom of the toilet bowl or sanitary napkins.
Using hygienic tampons, it is impossible to inadvertently remove a device. The IUD cannot get tangled or catch on a swab.
Signs that your IUD has fallen out include:
- Unusual vaginal discharge;
- Cramping and severe pain;
- Bleeding;
- Complaints of a partner (irritated tip of the penis);
- Pain during intercourse.
Symptoms that indicate the presence of infection (fever, unusual bleeding, colic, pain in the pelvic area) should make you consult a gynecologist immediately.
When should an IUD be inserted?
This is mainly done before ovulation or at the very end of menstruation. It all depends on the doctor and his/her skill.
Those doctors who prefer to insert an IUD during or immediately after the end of menstruation believe that the cervical passage during this period is slightly ajar, which allows inserting a device with less pain.
The IUD insertion is usually done 2-3 months after the childbirth. If you had an abortion or delayed period, the device is inserted a month later.
What are the advantages of an IUD?
- It provides very effective and permanent protection against unwanted pregnancy from the very moment of its insertion;
- It slightly affects the natural hormonal balance of the body;
- It allows you to have a carefree sex life: there is no need to not take birth control pills, use spermicidal capsules and ointments, measure body temperature;
- It facilitates the process of familiarization with the genitals since it requires constant fingering;
- You do not need to change the IUD often. Plastic IUDs should be changed every 3-4 years in order to prevent and exclude inflammatory processes of the pelvic organs;
- If you wish, you can conceive immediately after removing the IUD.
IUDs with copper wire are also changed every 3-4 years. They probably lose their reliability after this period since the starting oxidative processes do not allow copper ions to be active. And sometimes copper is simple – it simply dissolves and is absorbed by the body when it is deficient. IUDs containing progesterone last for a year.
What are contraindications to IUDs?
Absolute contraindications:
- Pregnancy;
- Acute or chronic genital infection;
- Underdeveloped uterus;
- Unreasonable bleeding from the genital tract of unknown origin;
- Postpartum period (recent birth).
General contraindications:
- Coagulation problems (poor blood coagulation);
- Cardiovascular diseases;
- Diabetes.
Relative contraindications:
- Fibroma;
- A woman who has not given birth (an IUDis placed only after the consent of a woman who has been warned about the possible consequences, and only if there is a complete ban on the use of contraceptive hormonal drugs). The patient’s condition is constantly monitored;
- Some malformations of the uterus;
- Previously performed operations on the uterus (scarring);
- Ectopic pregnancy or plastic surgery on the uterine lips in the past.
After IUD insertion care
Fortunately, a woman with an IUD inserted gets pregnant very rarely. If your period is delayed, get a pregnancy test immediately.
If the result is positive, undergo an ultrasound examination to determine the location of the IUD in relation to the uterine cavity and the embryonic sac.
If the device is under the embryo sac and the pregnancy proceeds normally, the gynecologist can carefully remove it to avoid infectious complications (this, of course, applies to women who want to continue the pregnancy).
If the device is located above the embryo sac, you must leave it in place and ensure the normal course of pregnancy. It is necessary to make an appropriate entry in the patient’s medical record so as not to forget to remove the IUD after delivery from the placenta.
One midwife even witnessed a newborn child hold-ing an IUD in his small fist grip. And finally, if a woman does not want to maintain a pregnancy, she can resort to its artificial termination.
Cases of spontaneous miscarriage in early pregnancy are most common. Cases of ectopic pregnancy account for 2.9%. This is a very serious and dangerous complication. If it is not detected on time, then a hole appears in the fallopian tube, then its rupture (the fallopian tube is too narrow to accommodate the growing egg), after which bleeding opens, inflammation escalates, infection occurs and, as a result, the tube is lost, which leads to infertility, and sometimes (in the past) to death.
Symptoms are the same as in early pregnancy (fatigue, vomiting, chest pain). Sometimes there are incessant blood-red discharge of black color, absence of menstruation, pain in the abdominal cavity of varying degrees of intensity (mild, dull, cutting), which increases with the development of pregnancy.
One or all of these symptoms occur suddenly, and therefore it is necessary to be very careful and consult a doctor as soon as possible. An ectopic pregnancy is a “bomb” inside that bursts at any moment.
Perforation most often occurs during the insertion of the IUD due to a doctor’s awkwardness or lack of experience. A poorly installed device abuts against the wall of the uterus, while part of the device half passes through the mucous membrane of the uterus or the device gets into the abdominal cavity.
What happens next? The device can move from organ to organ and penetrate into them, which requires urgent surgical intervention. Unfortunately, perforation does not have any particular symptoms that would allow it to be detected.
Therefore, too short strings or a complete absence during self-examination can serve as the first signal of concern. The second sign of perforation is pregnancy. As soon as the device has disappeared, the woman is no longer protected.
So, if the strings of the IUD are not groped and imperceptible when viewed with a mirror, then either the device fell out or perforation occurred. The doctor has a number of tools for a more accurate determination.
The specialist can examine the uterine cavity using a probe or a biopsy instrument. It is necessary to undergo fluorography (all plastic IUDs are covered with barium so that they can be detected using x-rays), and even better – sonography.
If the device is still in the uterus, you can pull on the strings to get it out. If the device has settled in the abdominal cavity, it must be removed since there is a danger of infectious disease, as well as difficulties in the functioning of organs that collide with the device, which leads to tingling and even pinching (for example, the intestines).
In such a situation, surgical intervention is required. The operation is often performed using endoscopy of the abdominal cavity. Inflammatory processes of the uterus and pelvic organs are the most common complications that in the future will affect the full functioning of the reproductive organs.
On average, when using an IUD, this danger increases 3 times; 7 times if a woman has not given birth; 1.7 times if she already has more than three children. For this reason, many doctors refuse to insert IUDs to young women who do not have children and have irregular sex lives with several partners, which increases the risk of infection or sexually transmitted viruses.
The prospect of entering a period of sexual maturity with an infection of the fallopian tubes, which ultimately leads to complete infertility, cannot satisfy either the doctor or the patient herself.
There are cases when the uterine mucosa accumulates around the IUD partially covering it, which does not allow the device to perform its functions. Removing the encapsulated IUD is very painful, sometimes you have to resort to curettage.
What are the disadvantages of an IUD?
Cons of using an IUD are not systematic and are completely absent in most cases. Nevertheless, under certain circumstances, a woman may feel inconvenience. During the IUD insertion, the rupture of the cervix with forceps is impossible if all actions and stretching are performed carefully. In case of damage to the cervix, it is treated immediately. Perforation of the uterus is a very serious complication since it is painless and cannot be detected immediately. Perforation occurs with inaccurate hysterometry or with the careless introduction of a device. In case of complications, a woman needs rest, ice on her stomach and a course of antibiotic treatment.